Summary
Quality Indicators (QIs) measure aspects of service provision that contribute to the quality of care given by residential aged care services (RACS). Participation in the National Aged Care Mandatory Quality Indicator Program (QI Program) has been a requirement for all Australian Government subsidised RACS since 1 July 2019. Data under the QI Program are collected and reported by RACS quarterly.
This quarterly report includes QI measurements from data collected from 1 April to 30 June 2025 for 2,560 RACS conducted under the QI Program (National Aged Care Mandatory Quality Indicator Program Manual 4.0). These RACS are those that had received Australian Government subsidies for delivering care, services, and accommodation in that period; and had submitted QI data by the submission due date (21 July 2025) up to the date of data extraction. Processing, checking, and preparing the data for transfer was completed by the Department of Health, Disability and Ageing between the submission and extraction dates, and was supplied to the Australian Institute of Health and Welfare (AIHW) on 4 August 2025.
Available data represented 98.5% of the 2,599 RACS that received government subsidies in the quarter (based on occupied bed days data extracted on 4 August 2025). Further detail on the care recipient coverage of the QI Program in this quarter, including counts of care recipient measurements and exclusions for each QI, is presented in Table S1 of the Technical notes.
It should be noted that the National Aged Care Mandatory Quality Indicator (QI) Program introduced new staffing QIs – covering enrolled nurses, allied health professionals, and lifestyle officers – starting from 1 April 2025. However, these QIs are not included in the Q4 (April–June) 2024–25 report due to their early stage of implementation, with further refinement and validation needed before formal reporting begins.
Definitions of quality indicators
A pressure injury is a localised injury to the skin and/or underlying tissue usually over a bony prominence, because of pressure, shear, or a combination of these factors. Assessment of pressure injuries in eligible care recipients is made on or around the same time and day in each quarter of the year. This can be done as part of the care recipient’s usual personal care. Consent is sought from care recipients before a full-body observation assessment is undertaken.
Eligible care recipients with one or more pressure injuries are reported against each of the six pressure injury stages:
- Stage 1 pressure injuries: intact skin with non-blanchable redness of a localised area
- Stage 2 pressure injuries: partial-thickness skin loss presenting as a shallow open ulcer with a red/pink wound bed
- Stage 3 pressure injuries: full-thickness skin loss, no exposure of bone, tendon or muscle
- Stage 4 pressure injuries: full-thickness loss of skin and tissue with exposed bone, tendon or muscle
- Unstageable pressure injuries: full-thickness skin tissue loss in which the base of the injury is covered by slough (yellow, tan, grey, green or brown) and/or eschar (tan, brown or black)
- Suspected deep tissue injuries: purple or maroon localised area of discoloured intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear
Additional reporting: Eligible care recipients with pressure injuries that were acquired outside of the service during the quarter are counted separately but are still included in the total number of care recipients reported as having pressure injuries.
The Quality of Care Principles 2014 (Quality of Care Principles) define restrictive practices as any practice or intervention that has the effect of restricting the rights or freedom of movement of a care recipient.
Restrictive practices QI measures and reports data relating to all restrictive practice, excluding chemical restraint. This includes physical restraint, mechanical restraint, environmental restraint, and seclusion.
It is a legal requirement for RACS to document all instances of restrictive practice (see Part 4A of the Quality of Care Principles). For this QI in each quarter, three days of existing records for all eligible care recipients at a service are assessed for any instances of restrictive practice (excluding chemical restraint). This QI is therefore a measure of the use of restrictive practices across the three-day period only. This three-day period is selected and recorded by services but must be varied each quarter and not known to the staff directly involved in care.
Restrictive practices are still recorded even if a care recipient or their representative has provided consent to the use of the restrictive practice.
Additional reporting: Eligible care recipients who were subject to the use of a restrictive practice exclusively through the use of a secure area are counted separately but are still included in the total number of care recipients who were subject to the use of a restrictive practice.
Weight loss is considered to be unplanned where there is no written strategy and ongoing record relating to planned weight loss for the care recipient. Eligible care recipients are weighed each month around the same time of the day and wearing clothing of a similar weight (e.g., a single layer without coats or shoes). Consent is sought from care recipients before an assessment on their body weight is undertaken.
This QI includes two categories:
- Significant unplanned weight loss: Eligible care recipients who experienced significant unplanned weight loss of 5% or more when comparing their current and previous quarter finishing weights
- Consecutive unplanned weight loss: Eligible care recipients who experienced consecutive unplanned weight loss every month over three consecutive months of the quarter.
A fall is an event that results in a person coming to rest inadvertently on the ground or floor or other lower level. For a fall to meet the criteria of resulting in a major injury, the fall must result in one or more of the following: bone fractures, joint dislocations, closed head injuries with altered consciousness and/or subdural haematoma. Assessment for falls and major injury is conducted through a single review of the care records of each eligible care recipient for the entire quarter.
This indicator includes two categories:
- Falls: Eligible care recipients who experienced a fall (one or more) at the service during the quarter
- Falls that resulted in major injury: Eligible care recipients who experienced a fall at the service, resulting in major injury (one or more), during the quarter.
Assessment for polypharmacy is conducted through a single review of medication charts and/or administration records for each eligible care recipient for a collection date selected by the service every quarter. For antipsychotics, a seven-day medication chart and/or administration record review is conducted for each eligible care recipient every quarter.
This indicator includes two categories:
- Polypharmacy: Eligible care recipients who were prescribed nine or more medications as at the collection date in the quarter
- Antipsychotics: Eligible care recipients who received an antipsychotic medication during the seven-day assessment period in the quarter.
Additional reporting: Eligible care recipients who received an antipsychotic medication for a diagnosed condition of psychosis are counted separately but are still reported in the total number of care recipients who received an antipsychotic medication.
Activities of daily living indicate a person’s ability to move and care for themselves, and include management of personal hygiene, dressing, going to the toilet, and eating.
Assessment for activities of daily living is conducted using the Barthel Index of Activities of Daily Living (ADL assessment), a 10-item questionnaire completed by a staff member for each eligible care recipient once per quarter using existing knowledge, care records, direct observation, and talking to the care recipient. The timing of measurement is chosen at the discretion of individual services but is recommended to occur around the same time each quarter. The ADL assessment reflects the care recipient’s performance in the 24-48 hours prior to the assessment.
The total score on the current quarter ADL assessment is compared to the total score on the previous quarter’s ADL assessment. A decline in ADL assessment is defined as a decline of one or more points from the previous quarter to the current quarter.
Eligible care recipients who received a ‘zero’ score (indicating dependence in all areas) on both the previous quarter and the current quarter are included in the total number of people assessed for this QI.
Additional reporting: Care recipients with an ADL assessment total score of zero in the previous quarter.
Incontinence is the loss of bladder and bowel control and can lead to incontinence associated dermatitis (IAD).
Incontinence care is assessed using the Ghent Global IAD Categorisation Tool, which categorises IAD severity based on visual inspection of the affected skin areas. Assessment is conducted by a staff member for each eligible care recipient once per quarter, around the same time each quarter. The timing of measurement is chosen at the discretion of individual services.
Eligible care recipients with incontinence are recorded. Additionally, eligible care recipients who experience IAD are reported against each of the four sub-categories:
- 1A: Persistent redness without clinical signs of infection
- 1B: Persistent redness with clinical signs of infection
- 2A: Skin loss without clinical signs of infection
- 2B: Skin loss with clinical signs of infection.
- The proportion of care recipients meeting criteria for IAD is calculated only for those who are recorded with incontinence.
Emergency department presentations and hospital admissions are potentially preventable if care recipients have timely access to appropriate healthcare services.
Assessment for hospitalisation is conducted through a single review of care records for each eligible care recipient over the entire quarter.
The QI includes two categories:
- Emergency department presentations: Eligible care recipients who had one or more emergency department presentations during the quarter
- Emergency department presentations or hospital admissions: Eligible care recipients who had one or more emergency department presentations or hospital admissions during the quarter.
Approved providers of residential aged care services report the number of staff working in defined roles over the entire quarter.
The defined roles to be reported are:
- Service managers
- Nurse practitioners or registered nurses
- Enrolled nurses
- Personal care staff or assistants in nursing.
Approved providers report workforce data in three steps:
- Staff who worked any hours in each of these roles in the previous quarter
- Of those recorded at Step 1, staff employed in each of these roles at the start of the current quarter (i.e. those who worked at least 120 hours in the previous quarter)
- Of those recorded at Step 2, staff who stopped working in each of these roles during the current quarter (i.e. those with a period of at least 60 days in the current quarter in which they did not work).
This QI is the number and proportion of care staff in each category who stopped working for the provider between quarters, as an indicator of workforce turnover.
The consumer experience QI captures the care recipient’s rating of six key attributes of care quality: respect and dignity, supported decision-making, skills of aged care staff, impact on health and wellbeing, social relationships and community connection, and confidence in lodging complaints.
Assessment for consumer experience is conducted using the Quality of Care Experience-Aged Care Consumers instrument, a 6-item questionnaire completed by the eligible care recipient (where possible) or a person who knows them well and sees them regularly (where the care recipient is unable to answer on their own behalf due to cognitive impairment). ‘Self-completion’ is when a care recipient independently completed the questionnaire, while ‘interviewer facilitated completion’ is when a care recipient is assisted to complete the questionnaire (i.e. by reading out the questions and response options) by an interviewer. The interviewer may or may not be a service staff member. Proxy-completion is when the questionnaire is completed by a family member, informal carer, or formal carer who knows the care recipient well.
Assessment occurs once per quarter, around the same time each quarter. The timing of measurement is chosen at the discretion of individual services.
Responses are categorised as:
- Excellent consumer experience: where a care recipient scores between 22–24
- Good consumer experience: where a care recipient scores between 19–21
- Moderate consumer experience: where a care recipient scores between 14–18
- Poor consumer experience: where a care recipient scores between 8–13
- Very poor consumer experience: where a care recipient scores between 0–7.
The QI is the number and proportion of care recipients who rated their consumer experience as ‘Good’ or ‘Excellent’.
The quality of life QI captures the care recipient’s perception of their position in life taking into consideration their environment, goals, expectations, standards, and concerns. Assessment examines independence, mobility, pain management, emotional wellbeing, social relationships, and leisure activities / hobbies.
Assessment for quality of life is conducted using the Quality of Life – Aged Care Consumers instrument, a 6-item questionnaire completed by the eligible care recipient themselves or via an interviewer (where possible) or a person who knows them well and sees them regularly (where the care recipient is unable to answer on their own behalf due to cognitive impairment). ‘Self-completion’ is when a care recipient independently completed the questionnaire, while ‘interviewer facilitated completion’ is when a care recipient is assisted to complete the questionnaire (i.e. by reading out the questions and response options) by an interviewer. The interviewer may or may not be a service staff member. Proxy-completion is when the questionnaire is completed by a family member, informal carer, or formal carer who knows the care recipient well.
Assessment occurs once per quarter, around the same time each quarter. The timing of measurement is chosen at the discretion of individual services.
Responses are categorised as:
- Excellent quality of life: where a care recipient scores between 22–24
- Good quality of life: where a care recipient scores between 19–21
- Moderate quality of life: where a care recipient scores between 14–18
- Poor quality of life: where a care recipient scores between 8–13
- Very poor quality of life: where a care recipient scores between 0–7.
The QI is the number and proportion of care recipients who rated their quality of life as ‘Good’ or ‘Excellent’.
Among the 11 QIs detailed in this report:
- Nine QIs (1-9) measure adverse events, complications, or undesirable outcomes. Lower values in these QIs indicate better quality of care
- Two QIs (10-11) measure desirable outcomes relating to consumer experience and quality of life. Higher values in these QIs indicate better quality of care.
National data: variation over time
A trend analysis is conducted to examine variation over time in QI performance. For the trend analysis, data are pooled together for every eligible care recipient reported about in the quarter. Trends are examined based on sector level outcomes per quarter.
At each quarter, the number of care recipients who meet criteria for a QI is counted. These counts are then compared over time using a quasi-Poisson regression model. More detail about the quasi-Poisson regression model can be found in the Technical Notes.
The trend analysis included data from 16 quarters, from July–September 2021 to April–June 2025. As noted above, 11 QIs are included in the trend analysis.
Regarding QIs that measure adverse events, complications, or undesirable outcomes (i.e., lower values of these QIs indicate better quality of care), results show that:
- Over time there has been a statistically significant decrease in the proportion of care recipients experiencing one or more pressure injuries, restrictive practices, restrictive practice exclusively through the use of a secure area, significant unplanned weight loss, consecutive unplanned weight loss, falls that resulted in major injury, polypharmacy, antipsychotic medication use, incontinence, and in the proportion of workforce turnover.
- There has been a statistically significant increase in both ‘emergency department presentations’ and ‘emergency department presentations or hospital admissions’.
- Over time there has been no statistically significant change in the proportion of care recipients experiencing falls, a decline in their ADL score, or IAD.
Regarding QIs that measure desirable outcomes (i.e., higher values of these QIs indicate better quality of care), results show that:
- There has been a statistically significant increase in the proportions of residents reporting ‘good’ or ‘excellent’ consumer experience and quality of life.
National data
QI data are presented below at a national level. The table presents data for all eligible care recipients aggregated across all 2,560 included RACS. The boxplot that follows presents data for all eligible care recipients aggregated at the service level. For further information on boxplots, see ‘Interpreting boxplots’ below.
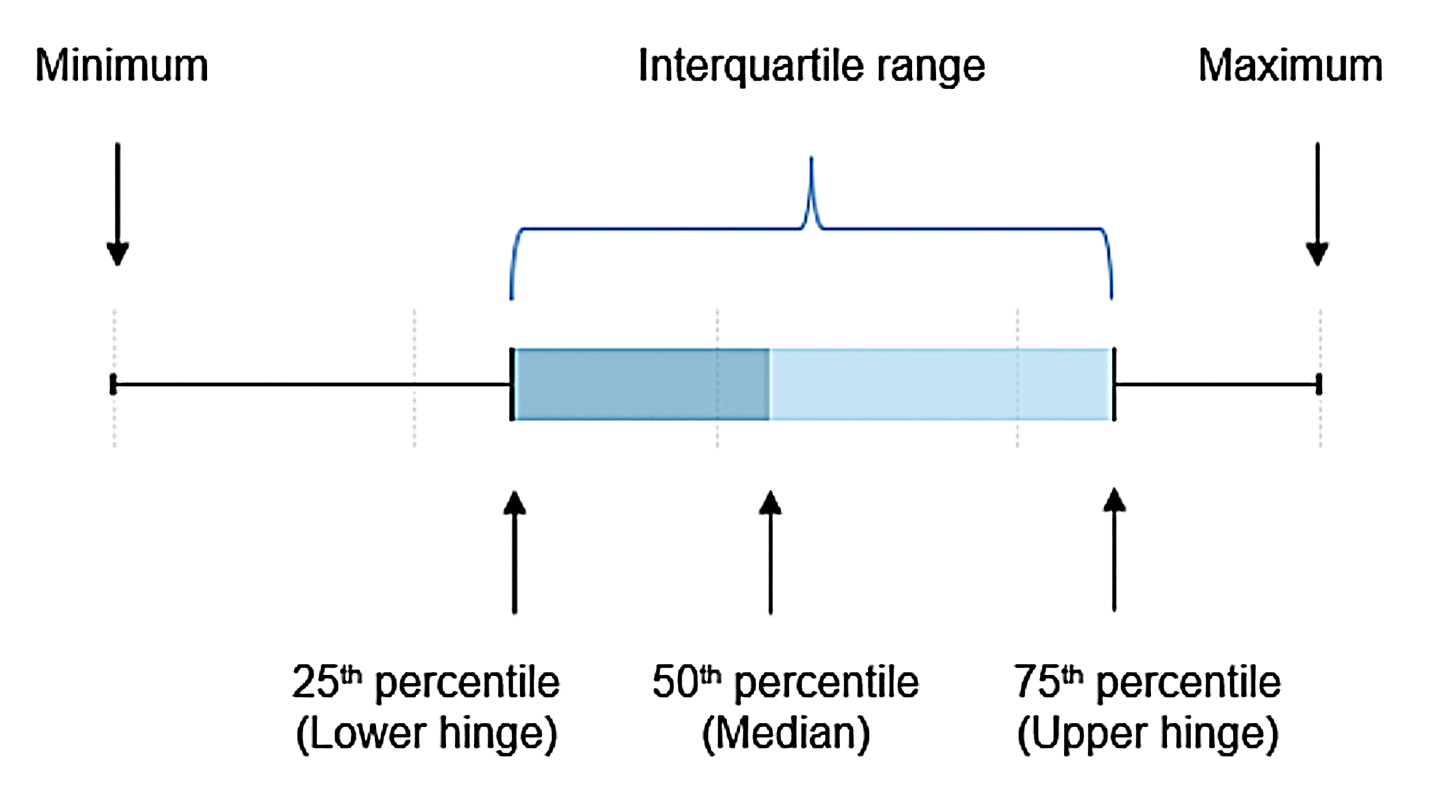
The values shown in the box plots are the minimum value, 25th percentile (‘Lower Hinge’), the 50th percentile (‘Median’), 75th percentile (‘Upper Hinge’) and the maximum value.
As an example of interpreting the percentiles, the 25th percentile shows at what QI prevalence rate 25% of the RACS reported a rate lower than this, and conversely 75% of the RACS reported a QI rate higher than this. The median value represents the QI prevalence rate in the middle of the values reported in Australia.
The interquartile range (IQR) is a measure of statistical dispersion or spread of QI rates and is the difference between the 75th percentile and the 25th percentile values.
.png)
Geographical variation
Disaggregations of QIs by state and territory and by remoteness categories were calculated from raw data with no risk adjustment. At the time of reporting, it is not possible to take into account variation in the complexity of people’s care needs at the service level (case-mix) nor how this interacts with other features known to vary across geographical areas, such as service size, service ownership or interaction with healthcare services (such as hospitals and palliative care services).
Technical notes
Notes
Amendment
14 October 2025 – Data in rows 47–61 in Tables 3.1 and 3.2 in Data tables – 1 April to 30 June 2025 published on 3 October 2025 have been restructured. This does not impact the numbers reported in the main report.

